LASIK and PRK vs REFRACTIVE LENS EXCHANGE (RLE) FOR VISION CORRECTION
In patients who are in their mid-50s or older, the question often comes up whether to correct vision by LASIK or by refractive lens exchange (RLE). LASIK involves reshaping the outter side of the cornea with an extremely precise laser beam and does not enter into the inside of the eye. RLE, on the other hand, is essentially cataract surgery, but before there is an actual cataract. A cataract is a clouding up of the natural lens of the eye, which sits inside the eye behind the pupil. When the lens of the eye becomes cloudy, the only treatment we currently have is to go inside the eye surgically and remove the lens. A clear plastic replacement lens called the “implant” is then inserted permanently inside the eye in place of the natural lens. The patient’s prescription can be built into this implant so that the vision can be corrected at the time of cataracts surgery, which is an extra benefit. Certainly, when someone has a cataract, this is the best way to handle the situation. The question comes up, though, about removing the clear natural lens before it gets a cataract and replacing it with an implant to correct vision. Performing cataract surgery before there is a cataract is called refractive lens exchange or RLE.
ADVANTAGES OF REFRACTIVE LENS EXCHANGE (RLE) OVER LASIK
Proponents of RLE point out that if one has RLE instead of LASIK to correct vision, then the patient never will develop a cataract since the natural lens will already have been replaced by the plastic implant and plastic implants cannot get cataracts. Proponents would argue that patients in their mid 50-s or older already have natural lenses that have become stiff through presbyopia, causing the need for reading glasses or bifocals (a “dysfunctional lens”). Removing and replacing an older lens that does not function as well as a younger lens, they would argue, is more reasonable than removing a fully functional, flexible lens in a 30 year old, for example, who is too young to have developed presbyopia. Furthermore, there are now implant technologies that can correct presbyopia, although they do not do so perfectly. These would include multi-focal and extended range of focus lenses, both of which have their own pros and cons. If a patient in their mid-50s or older has LASIK, the lens of the eye still will eventually develop a cataract (as it would have anyway) if the patient lives long enought and the patient will eventually need cataract surgery anyway. Proponents of RLE argue that lens replacement in the mid-50s “kills two birds with one stone”.
ADVANTAGES OF LASIK OVER REFRACTIVE LENS EXCHANGE (RLE)
There are, however, significant arguments in favor of doing LASIK or PRK rather than RLE in a patient in their mid-50s or older, until the age a cataract actually does develop. The first argument is that RLE is significantly more invasive than LASIK, or PRK. RLE enters inside the eye, whereas LASIK or PRK stay outside the eye. This makes the risk of RLE signficantly higher than LASIK or PRK. And, even more worrisome, several studies have shown an permanent increase in yearly risk of retinal detachment after lens replacement surgery with many studies suggesting a risk rate of 1% to 2% chance of retinal detachment per year. Retinal detachment is a very serious medical condition which can even be blinding. So the risk of RLE is higher at the time of surgery and also after surgery is completed, for the rest of the patient’s life. RLE also is less accurate than LASIK or PRK. Certainly, cataract surgery can be performed after LASIK or PRK when the patient finally does develop a cataract. In fact, the accuracy of cataract surgery after LASIK or PRK is rapidly increasing due to the recent FDA approval of the light adjustable lens.
A NEW CONSIDERATION: RAPIDLY IMPROVING PRESBYOPIA-CORRECTING LENS IMPLANT TECHNOLOGY WORTH WAITING FOR
Now a new consideration has entered the decision between LASIK and RLE. If a patient has lens replacement now, before a visually significant cataract has developed, the implant that will be inserted will reflect contemporary technology – and it is very difficult to ever change that lens later for newer technology. Essentially, by having catarct surgery before it was necessary to do so, the patient is prematurely “locking” themselves into current lens implant technology and missing the opportunity to have a much more advanced implant put in the eye down the road if they waited to have lens replacement until it was necessary due to actual cataract development. Having LASIK now instead of RLE allows the patient to enjoy improved vision without the increased risk and decreased accuracy of RLE — and allows the patient to wait until cataract surgery is actually necessary, which could be decades down the road.
The logic of deferring catarct surgery rather than jumping into lens replacement surgery became even more compelling with the recent announcement of an entirely new lens technology which hopefully will finally mimic the natural lens’s ability to flex to change its shape and allow reading vision equivalent to a 20 year old. This could be a lens worth waiting for.
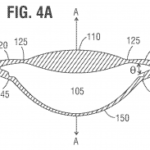
Earlier this year, at the annual meeting of the American Society of Cataract and Refractive Surgery, data was presented for the Juvene Intraocular Lens. This impant is a breakthrough design that uses fluid shifts to allow the front surface of the lens to change shape within the eye. A 4 year study, the GRAIL study, showed good vision over a wide range of distances, from near to far, after it was implanted. The company that developed this lens implant hopes to begin FDA clinical trials early next year. If this lens, or a lens similar to it, can be proven to be safe and durable inside the eye over time, it will be a game changer for lens replacement surgery and make reading glasses no longer necessary. It will also be optically superior to current presbyopia-correcting lens implantdesigns such as multi-focal or extended range of focus implants.
MY PERSEPCTIVE ON LASIK vs RLE
My personal bias is to consider lens replacement surgery a “can to be kicked down the road” as long as possible — until one acctually develops a catarct. Given the lower risk and higher accuracy of LASIK or PRK — and given the exciting developments on the horizon with lens implant technology — I think it is very reasonable to improve vision with LASIK or PRK now and take care of cataracts when they develop, which hopefully will be far into the future. There is no rush to do surgery inside the eye. If a patient comes to see me with trivial levels of lens change, this is the message I give them. If they have more advanced lens changes and it looks like cataract surgery will be required in the near to mid-term future, then I think it is reasonable to jump ahead a bit and have RLE. If a patient actually has a visually significant cataract that is limiting their vision, then cataract surgery is the best option. Of course, no one has a crystal ball and sometimes lenses that look clear can rapidly develop into cataracts and sometimes the opposite is true, namely lenses that look like cataract surgery is just around the corner can show little change for many years. Ultimately, the choice between LASIK and RLE is up to the patient and my job is to help the patient understand that status of their lens and the pros and cons of their options, including RLE vs. LASIK.